Is your physician practice’s schedule a bit lighter than you’d like? This article examines some of the top overlooked areas that can cause physician practices to lose patients and damage the overall patient volume. The goal is to help inspire practices that may have lost their way and refresh those who want to stay “on their toes”.
This is part 1 of 2, which focuses on the areas relating to scheduling and the patient experience. Part 2 will focus on reputation, relationships, and referrals. Let’s dive in!
- Patients continue to become accustomed to increasing levels of convenience in their lives.
- Over 68% of patients want to schedule appointments and communicate with their doctor online. It can not only keep patients happy, but also make offices more efficient.
- Calls should be answered quickly, with minimal wait, and not have to leave a message.
- Minimize wait time for appointments, with same or next day appointments being the ideal.
- Having reminder calls are a start, but are not what most patients want and are not the most effective method.
- Effective and accurate return visit and recall processes ensure patients return to care at the recommended intervals.
- Stagnation or complacency can destroy a practice, so develop a strong culture that encourages growth and continuous improvement, to ensure long-term success.
The Importance of Convenience
Most of us would agree that Americans love convenience. From fast food to online shopping with items shipped right to our doors, we love it. When fast food became too inconvenient, an app was created so it could be brought right to us. As we become accustomed to this level of convenience, it shouldn’t be a surprise when patients start to expect the same from their healthcare providers.
A commonly overlooked and highly undervalued area is that of patient convenience. Many practices simply make it too inconvenient for patients to schedule an appointment. Meanwhile, there are several healthcare startups offering a variety of different apps and telemedicine services. Retail healthcare continues to grow, and some unexpected specialties are predicted to be a part of it (ex. Oncology). Traditional physician practices who fail to evolve may see their patient population poached and the bottom line erode in the near future.
Practices can utilize the “Golden Rule” as a rough guide when determining if an area is not patient-centric. For example, if you personally would not want to wait on hold for 5 minutes, it’s a reasonable assumption that at least some patients may not want to either. While convenience is highly subjective, the more objections eliminated, the more likely patients are to schedule.
Not Using Patient-Facing Technology
When considering the extent that we utilize and rely on technology in our everyday lives, is it surprising that consumers would expect it? It is truly amazing how much technology has changed in the past few years and the rate which it gains general acceptance. Not that long ago the idea of ordering things online was high-tech. Since then, we’ve had the smartphone app revolution, and most recently have been introduced to ordering on smart watches and voice activated virtual assistants. While some providers have invested in technology heavily, even in 2020 we have some without a basic website.
A 2019 study by Accenture shows a significantly increasing patient demand for electronic communication with their physician’s office (ex. scheduling, portal, messaging, and lab results). When participants were asked if the capability of booking/changing/cancelling appointments would “increase your likelihood of choosing that provider“, 68% indicated it made them “more likely” or higher. Of these responses, “Much more likely” ranged from 40% for millennials to 18% for the silent generation.
A properly implemented, well designed technology solution should increase the overall efficiency of the practice. These savings can be utilized to provide more phone coverage, decrease staffing expenses, or focused on areas with much greater financial impact for the practice.
While these are excellent tools, they are not just something that can be purchased and forgotten about. The physicians and staff must be trained, it must be incorporated into workflows and utilized consistently throughout the day, and patients need to be encouraged to utilize it. The setup must be done correctly and all applicable features utilized to maximize the benefit.
Historically some practices have cited cost and interfacing difficulties as roadblocks, however there are now more third-party options than ever before. In the worst-case scenario, there are standalone products available that do not require a full integration with the EMR. It’s still possible to gain many of the benefits despite many technological limitations faced.
Practices that do not use patient-facing technology will likely find themselves competing for smaller and smaller slices of the pie. Consider implementing technology as a goal for this year.
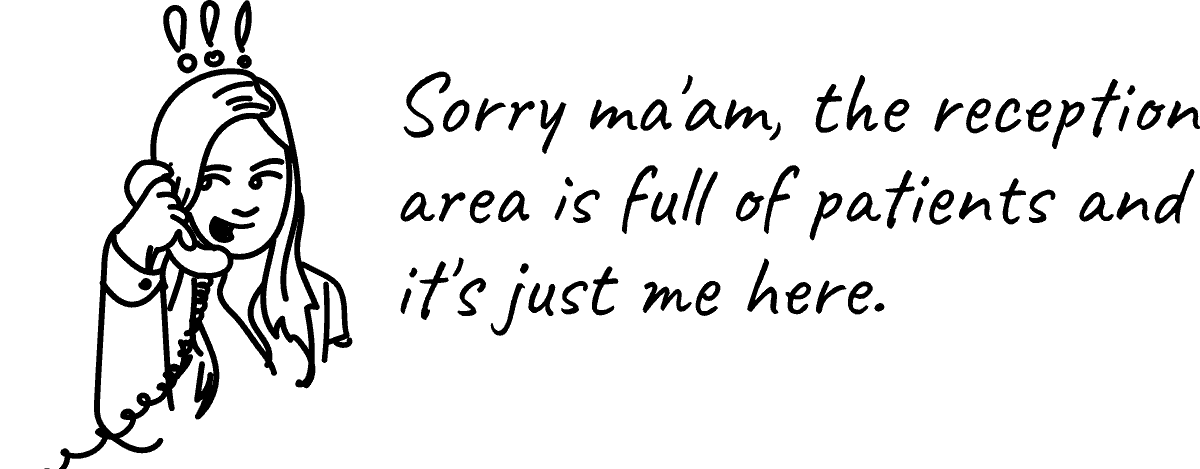
Neglecting the Phones
Regardless whether a practice has implemented technology solutions, it is still extremely important to be mindful of the phones. These calls are often more time sensitive than requests received from other communication routes, such as clinical concerns and referring providers trying to send patients. When urgently seeking assistance, it’s only normal to be even less patient. While we hope that they call back later, the truth is that it is not always the case.
Established patients may opt to forgo an appointment altogether or try utilizing a retail medical clinic, urgent care, or emergency room. Apps and telemedicine will likely soon be on that list as well. While missing a few visits may not seem important, these same patients may just like the convenience and not come back permanently.
A good goal for many practices may be: answering calls within 20 seconds, minimizing the hold time, and having none go to voicemail (during business hours). Unfortunately, many practices find it difficult to reach anywhere near this. Most phones in physician practices are actually very sophisticated and just not configured to their fullest potential. Most have the ability to provide detailed information that can be used to gain insight into the performance of a practice and identify areas for opportunity.
Due to the vast differences between practices, what works well in one practice may make the situation worse in another. If this is an area of concern, it may be worthwhile considering a consultant that understands both the phone system and physician practice workflows in order to suggest changes while minimizing impact. They will also be able to help leveraging some of the other advanced features in the phone system to enable staff to manage calls more efficiently.

First Available Appointment Isn’t Soon Enough
The topic of first availability is often a sensitive subject. When an established patient has a concern that they believe needs urgent attention, failing to accommodate can make some patients feel they are not valued. As with the previous topics, these too may forgo an appointment or seek more convenient care options.
With new patients, while some may find an appointment two weeks away to be perfectly acceptable, others may be adamant that tomorrow is too far away. When a patient thinks they can potentially be seen sooner, it’s not uncommon for them to “shop around”. While this may not sound too bad, some practices inadvertently turn away a very significant amount of patient volume each month.
When asking physicians about their first availability, I frequently hear that they would be willing to see someone that same day. Then, minutes later, hear patients told something else by the staff. Typically, it doesn’t take much more than asking a few questions or observing those patient interactions to hear what is really being conveyed. Whether from a communication gap, training opportunity, process problem, or something else, these scenarios can often be resolved quickly with fairly drastic results.
While it won’t be possible to accommodate every patient, there are often opportunities to “tweak” the physician’s schedule and associated workflows in order to strategically increase availability. In addition to those tweaks, some basic strategies utilized by practices are:
- Reserving specific slots – dedicated to these time-sensitive appointment types each day. Allow staff to begin scheduling patients from the wait list into those slots at a certain point in the day.
- Seeing them as a walk-in – the patient can be notified that although the schedule is extremely full, if they don’t mind waiting a bit, they can come in to fill out paperwork and will be brought back as soon as an opportunity opens up.
- Having a wait list – while they don’t solve the underlying problems, they do help the practice to quickly fill last minute cancellations and enable some patients to be seen sooner.
A frequently heard complaint from staff is being scared to double book or add on patients after being told to “use their best judgment” and the results not been as the physician expected. Often, staff actually prefer having a written policy/guide, because it provides straightforward guidance on handling these situations.
Did you know, certain payers in Texas (especially HMO’s), have explicit access to care time-frames required of contracted providers? Many require providers to do certain things if they are ever unable to meet these. Depending on specialty and reason for visit, the time-frames can be sooner than you may think, so it’s important to be aware of them.
Reminders & Return Visits & Recalls
Equally important to getting the initial appointments made are ensuring that they and future appointments are kept. Many practices struggle with these as they are very time consuming. However, they are essential to maintaining a practice’s patient volume.
These areas are also highly impacted by the previously discussed ones. For example, if staff is already struggling to keep up with the phones, the last thing we would want to do is direct a large amount of patient reminders to be sent at that time. Conversely, by actively managing the processes, the practice can plan for the patient volume ahead of time and strategically spread the appointments out or push them towards ideal days of the week.

Reminders
Appointment reminders are a tool that’s been repeatedly shown to reduce no-show rates. While these won’t eliminate the issue completely, for practices that are not part of the 88% currently utilizing them, now may be a good time to consider it. While reminders can’t ensure patients keep their appointments, they increase the likelihood of keeping the appointment and maximize the amount of advanced notice when cancelling. This gives practices additional time to attempt to fill the slot.
If staff is currently placing reminder calls manually, adding the ability to have text messaging (SMS) and email incorporated, may be beneficial. Many recent studies show not only do patients prefer text messages and email to phone calls, they also result in lower no-show rates. Several sources suggest that two or even three+ specifically time reminders are significantly more effective than a single reminder. There is also an argument to be made for utilizing a combination of voice, text, and email to ensure receipt.
Practices should ensure patients are aware of the practice’s cancellation policy to further encourage keeping scheduled appointments. This is not to suggest that practices should or should not charge a fee, just that patients be made aware of how many hours’ notice that they should provide if unable to attend.
Recalls & Returns
In most specialties, there are three common scenarios where patients are asked to come back in to the office (and frequently do not). These are:
- Return for treatment based on imaging, lab work, or outside records.
- Follow-up on acute problems and conditions
- Routine preventive care (such as annual wellness visits, monitoring of chronic conditions, or monitoring of high-risk patients)
Having organized processes in place to ensure these patients return at the appropriate times is not just good for the patients’ well-being, but helps to ensure a steady patient volume. Some best practices may include things like:
- Ensuring patients have an appointment for their next visit prior to leaving the office.
- Ensuring the appropriate Return to Care (RTC) times are recorded in the chart, ideally in a way that reports can be run to identify anyone that’s non-compliant.
- Incorporating a mixture of technology and people into the processes to maximize efficiency while limiting the chance of human error. This could be as simple as a couple automated attempts followed by human ones.
- If at all possible, structure these processes so that at least a second person (ex. supervisor, manager, nurse, or physician (as appropriate)) must sign-off before a patient can be removed from lists or a chart marked inactive, this allows a second set of eyes to confirm all appropriate efforts have been made.
Unfortunately, many EMRs are not capable of or not configured in a way that makes tracking these easy. They often make it very easy for a single wrong click to cause a patient to “fall off the radar” completely unnoticed. A carefully designed process will help to ensure patients return as appropriate.

Preventing Future Recurrence
Some general tips that may help a practice to proactively address many of these areas are:
- Ensuring the practice maintains a patient-centric focus will help prevent it from veering off course.
- Don’t allow the practice to become “content” with the status quo. Processes should be routinely reviewed to ensure effectiveness and identify opportunities for improvement.
- Keeping in mind, the majority of patients that have a poor experience will not say anything to the practice, however, will often tell friends, family, a social network, or a review site all about it. The reach of such, being far further than just that one patient.
- Expecting the unexpected. In addition to the normal day-to-day scenarios, processes should also address the other scenarios that may occur. This will help ensure the intended outcomes.
- Regularly reviewing practice performance data. It’s essential to have effective high-level reports and/or dashboards to efficiently and effectively monitor practice performance at a glance, so that course corrections can be made nimbly.
- Building a great team in a practice culture that encourages creative problem solving, empowerment, and collaboration can pay off in many ways, including having a full team of people that look out for the well-being of the practice, rather than just one or two.
- Considering the overall benefit of bringing in a professional to help diagnose problems quickly and minimize the overall financial impact they may cause.
Be sure to follow us on Facebook, Twitter, or LinkedIn for part two of this article which will look at reputation, relationships, and referrals!